Asthma
Definition of asthma
- Chronic inflammatory disease of the airways
- 3 components:
- Reversible and variable airflow obstruction
- Airway hyper-responsiveness to stimuli
- Inflammation of the bronchi
Epidemiology of asthma
- Increasing prevalence – estimates of prevalence range from 3 to 5.4 million
- Approximately 235 million people worldwide affected
- Approximately 250,000 people die per year from the disease
Aetiology of asthma
- Atopy and allergy – pets, pollen
- Cold air
- Exercise
- Pollution
- Occupational
- e.g. isocyanates (paint sprayers), latex, flour and grain dust
- Viral infections
- Drugs
- e.g. NSAIDs, Beta blockers
- Emotion
Presentations of asthma
- Cough
- Wheeze
- Breathlessness
- Chest tightness
- Features which increase the probability of asthma include:
- Diurnal variation (worse at night and early morning)
- Triggered by or made worse by above aetiologies
- Recurrent and frequent symptoms
- Family history of atopy or asthma
Differential diagnosis of asthma
- Respiratory
- Churg-Strauss
- Look for high eosinophils
- Allergic bronchopulmonary aspergillosis
- Allergy testing for common moulds
- COPD (exacerbation)
- Chronic cough syndromes
- Rhinitis
- Bronchiectasis
- Sarcoidosis
- Lung cancer
- Churg-Strauss
- In chidren
- Croup and epiglottitis
- Obliterative bronchiolitis
- Cystic fibrosis/ Ciliary dyskinesia
- GORD
- Heart failure
- Tracheomalacia
- Narrow trachea on bronchoscopy, obstructive picture on spirometry
- Vocal cord dysfunction
Investigation of asthma
- Peak flow charts
- Lung function tests
- FEV1/FVC <0.7
- Reversibility/ improvement after treatment trial
- CXR
- In patients presenting atypically or with additional symptoms or signs
- Tests of atopy
- Skin prick testing
- Blood eosinophilia
- Raised specific IgE
- Further investigations
- Methacoline PC20 – the provocative concentration of methacholine required to cause a 20% fall in FEv1. .
- FENO – Exhaled NO concentration
- Indirect challenges – e.g. exercise challenge
- Sputum eosinophil count
- In acute asthma (see Acute Asthma pages for full details on acute asthma)
- CXR
- Recommended in the presence of suspected pneumothorax, consolidation, life threatening asthma, requirement for ventilation, failure to respond to treatment
- Pulse oximetry
- ABG
- CXR
It is important to obtain objective support for the diagnosis of asthma given the potential long-term treatment implications. Repeated assessment and measurements may be needed. Whether or not this should happen before starting treatment depends on the certainty of the initial diagnosis and the severity of presenting symptoms.
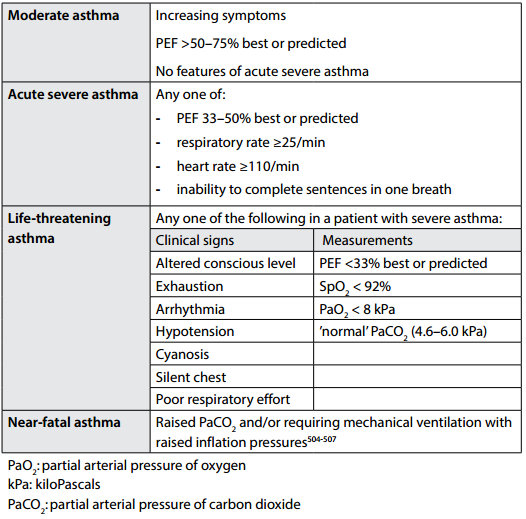
Staging of acute asthma (Table from BTS 2014 asthma guidelines)
Initial management of acute asthma (see Acute Asthma pages for full details on acute asthma)
- Oxygen: aim sats 94-98%
- Inhaled/Nebulised high dose Beta 2 agonists
- e.g. 2.5-5mg nebulised salbutamol at 15-30 min intervals
- Steroid therapy
- 40mg prednisolone po daily for 5 days. If oral route not possible – IV hydrocortisone 400mg daily or IM methylprednisolone 160mg daily.
- In patients failing to respond to initial treatment or with acute severe or life threatening asthma:
- Nebulised ipratropium bromide
- 0.5mg 4-6 hourly
- Magnesium sulphate
- 1.2-2g IV infusion over 20 minutes
- IV aminophylline
- 5mg/kg loading dose IV over 20mins (unless already on oral therapy), then infusion of 0.5-0.7mg/kg/hr.
- If on oral maintenance therapy – check level on admission
- Monitor levels whilst on infusion (Aim 10-20mg/l)
- Early referral to ITU. Indications include:
- Deteriorating PEF
- Persisting or worsening hypoxia
- Hypercapnia
- Fall in pH in ABG
- Exhaustion
- Reduced GCS
- Nebulised ipratropium bromide
Management of chronic asthma (See BTS 2014 asthma guidelines for full guidelines)
Non-Pharmacological
- Self-management plan
- Allergen avoidance
- Smoking cessation
- Immunisations
- Immunotherapy
Pharmacological: Stepwise Drug Treatments (see BTS/SIGN Guidelines) – move both up and down the steps
- Step 1: Reliever therapy
- Short acting beta-2 agonist as required: Salbutamol 100-200mcg
- Step 2: Regular preventer therapy
- Introduce inhaled steroid if: exacerbations in last 2 years; using salbutamol 3x/wk; symptomatic 3x/week; waking one night/wk
- Usual starting dose 200mcg bd (Budesonide – alternatives include beclomethasone and fluticasone)
- Step 3: Add-on therapy
- Trial long acting beta 2 agonist (LABA): Salmeterol 50mcg/12h
- If no response to LABA: stop LABA and increase inhaled steroid dose to 800mcg/day
- If some, but inadequate, response to LABA: increase inhaled steroid dose to 800mcg/day. And if still inadequate response consider alternative add-on therapy:
- Leukotriene receptor antagonist (first choice add-on therapy in children)
- Theophyllines
- Slow release beta 2 agonist tablets
- Step 4: Additon of a 4th drug
- If control remains inadequate, consider the following interventions:
- Increasing inhaled steroids to 2000 micrograms/day
- Adding 4th drug e.g. leukotriene receptor antagonist; theophylline; slow release β2 agonist tablets (caution in patients already on long-acting β2 agonists
- Step 5: Oral steroids
- Add regular oral prednisolone (at lowest dose for symptom control)
- Monitor for systemic side effects: BP, blood glucose, bone mineral density, cholesterol
- Continue high dose inhaled steroid
- Refer to specialist asthma clinic
- Add regular oral prednisolone (at lowest dose for symptom control)
- Other medications and potential steroid sparing agents (only for use by specialist centres):
- Anti IgE monoclonal antibody: Omalizumab
- Immunosuppressants (methotrexate, ciclosporin, gold)
Good asthma control can be defined as:
- No daytime symptoms
- No night-time awakening due to asthma
- No need for rescue medication
- No exacerbations
- No limitations on activity including exercise
- Normal lung function (in practical terms FEv1 and/or PEF>80% predicted or best)
- Minimal side effects from medication.
Complications of asthma
- Pneumonia
- Lobar collapse
- Pneumothorax
- Respiratory failure
- Side effects from treatment
- e.g. hypokalaemia, arrhythmias
- Fatigue
- Psychosocial problems: depression, difficulties at work
Markers of poorer prognosis in asthma
- Poor adherence
- Previous acute admissions and/or intubation
- 3+ different classes of asthma medication
- Psychosocial dysfunction
- Inadequately treated disease
- Smoking
Click here for medical student OSCE and PACES questions about asthma
Common asthma exam questions for medical students, finals, OSCEs and MRCP PACES
Click here to download free teaching notes on asthma: Asthma
Perfect revision for medical students, finals, OSCEs and MRCP PACES